Medizin - Zeit - das Gute Leben
Medicine - Time - the Good Life
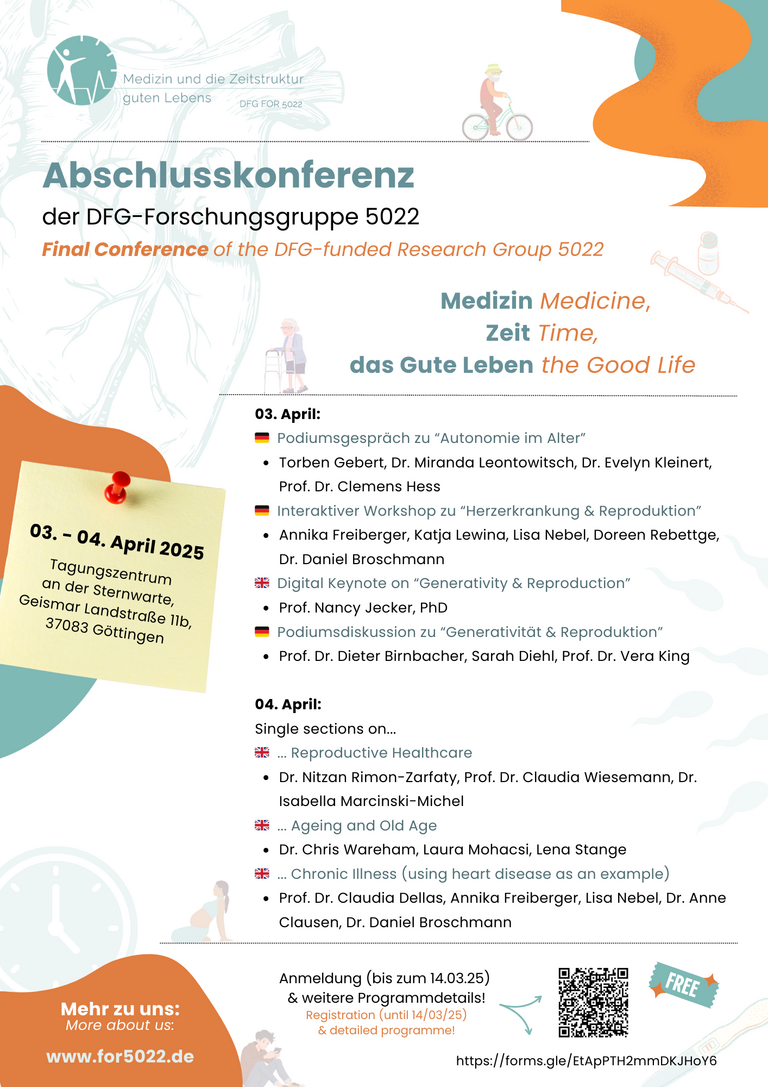
Nach vier Jahren intensiver Forschung endet im April 2025 die aktuelle Förderperiode der DFG-Forschungsgruppe „Medizin und die Zeitstruktur guten Lebens.“ In den Bereichen der chronischen Herzerkrankung, der Fortpflanzungs- und der Altersmedizin hat die interdisziplinäre Forschungsgruppe die ethische Relevanz menschlicher Lebenszeit für die Medizin herausgestellt. In einer internationalen Abschlusskonferenz am 3.-4. April 2025 im Tagungszentrum an der Sternwarte, Göttingen, stellen die Forschenden ihre Ergebnisse vor und laden in interaktiven Workshops zum Austausch ein.
Die öffentliche Konferenz beginnt mit einem Stakeholder-Workshop: Dieser thematisiert einerseits die Frage, wie Autonomie in den verschiedenen Phasen des Alterns gestaltet werden kann; andererseits werden die besonderen Herausforderungen in den Blick genommen, die sich jungen Herzpatient*innen stellen können, wenn sie über eine Familiengründung nachdenken. Betroffene und medizinisches Fachpersonal können hier niederschwellig mit Forscher*innen ins Gespräch kommen. Im Verlauf der Konferenz werden ethische Fragen chronischer Erkrankung, der Fortpflanzungsmedizin und des Alterns in Vorträgen und Podiumsdiskussionen weiter vertieft. Der erste Konferenztag wird auf Deutsch, der zweite auf Englisch abgehalten werden. Die Konferenz wird auch digital übertragen. Um Anmeldung bis zum 31. 03. 2025 wird gebeten.
Anmeldung:
Bitte informieren Sie uns über Ihre Teilnahme vor Ort oder digital, indem Sie folgendes Formular ausfüllen:
https://forms.gle/EtApPTH2mmDKJHoY6
Anmerkung: Das Formular wurde mittles der Software Google Forms erstellt und verlangt fälschlicherweise von manchen Nutzer*innen eine Google-Mailadresse. Dies scheint jedoch ein Problem des Browsers Firefox zu sein! Sollten Sie diese Meldung erhalten, wechseln Sie bitte den Browser oder wenden sich mit einer Mail an anna.kapp@med.uni-goettingen.de!
Beim Ausfüllen des Anmeldeformulars erhalten Sie auch die Möglichkeit, sich für unseren Newsletter anzumelden! Wenn Sie daran nicht interessiert sind, können Sie sich auch über den folgenden Registrierungslink direkt die Online-Teilnahme sichern!
uni-goettingen.zoom-x.de/webinar/register/WN_8Zhz_J3dRiCiuDrzDu4Lvg
Wir freuen uns auf Ihr Kommen!
Programmablauf:
Donnerstag, 03. 04. 2025
11.30 Offenes Ankommen mit Snackangebot
Teil 1: Stakeholder-Workshop (Deutsch)
12.00 Begrüßung und Einführung: Prof. Dr. Claudia Wiesemann (Universitätsmedizin Göttingen)
12.30 Autonomie im Alter: Wie verändern sich Vorstellungen von Autonomie im Prozess des Älterwerdens?
- Ein Podiumsgespräch mit Torben Gebert (Klinik für Palliativmedizin, Universitätsmedizin Göttingen), Prof. Dr. Dr. Clemens Hess (Seniorenbeirat Göttingen), Dr. Evelyn Kleinert (Universitätsmedizin Göttingen), Dr. Miranda Leontowitsch (Leiststelle Älterwerden, Frankfurt)
Moderation: Dr. Christian Hißnauer (Humboldt-Universität Berlin)
14.00 Pause/Break
14.30 Familiengründung und Herzerkrankung: Welche Fragen tun sich auf?
- Ein interaktiver Workshop mit Dr. med. Anna Dückelmann (Charité Berlin), Annika Freiberger (Deutsches Herzzentrum München), Katja Lewina (Freie Autorin), Lisa Nebel (Universitätsmedizin Göttingen), Doreen Rebettge
Moderation: Dr. Daniel Broschmann (Universitätsmedizin Göttingen)
16.00 Pause/Break
Teil 2: Generativity and Reproduction (Deutsch/English)
17.00 As Temperatures Rise, Should Birthrates Fall? A Parenting Ethics Response to Climate Change (digital)
- Keynote by Prof. Nancy Jecker, PhD (University of Washington School of Medicine)
18.00 Sollen wir aus Generativitätsgründen auf Reproduktion verzichten?
- Eine Podiumsdiskussion mit Prof. Dr. Dieter Birnbacher (Heinrich-Heine-Universität Düsseldorf), Sarah Diehl (Freie Autorin und Aktivistin), Prof. Dr. Vera King (Goethe Universität Frankfurt)
Moderation: Prof. Dr. Mark Schweda (Carl von Ossietzky Universität Oldenburg)
19.00 Ende des Tages/end of day one
Freitag, 04. 04. 2025
Teil 3: Sections (Englisch)
9.00 Reproductive Healthcare:
- Putting Reproduction on Ice: Navigating Temporality in Social Egg Freezing – A Comparative Study of Germany and Israel
Dr. Nitzan Rimon-Zarfaty (Universitätsmedizin Göttingen, Sapir Academic College)
- Reproductive Healthcare, Time, and the Good Life
Dr. Isabella Marcinski-Michel (Universitätsmedizin Göttingen), Prof. Dr. Claudia Wiesemann (Universitätsmedizin Göttingen)
Chairing: Ines Pietschmann (Universitätsmedizin Göttingen)
11.00 Ageing and Old Age:
- Cryonics And the Story of a Life: Closing the Book on the Frozen Dead
Dr. Chris Wareham (Utrecht University)
- Images of Old Age: Bioethics and Perspectives of Health Care Professionals and Seniors
Laura Mohacsi (Universitätsmedizin Göttingen), Lena Stange (Carl von Ossietzky Universität Oldenburg)
Chairing: Prof. Dr. Mark Schweda (Carl von Ossietzky Universität Oldenburg)
13.00 Pause/Break
14.00 Chronic Illness - Using Heart Disease as an Example:
- Chronically Ill With a Congenital Heart Defect. How the Advancements of Medicine Influence the Lives of Those Affected
Prof. Dr. Claudia Dellas (Universitätsmedizin Göttingen)
- Parenthood with Chronic Illness - The Importance of Generativity for the Quality of Life in Adults with Congenital Heart Disease
Annika Freiberger (Deutsches Herzzentrum München), Lisa Nebel (Universitätsmedizin Göttingen)
- Chronic heart disease and the future: the concept of existential possibility
Dr. Daniel Broschmann (Universitätsmedizin Göttingen), Dr. Anne Clausen (Georg-August-Universität Göttingen)
Chairing: Dr. Daniel Broschmann (Universitätsmedizin Göttingen), Lisa Nebel (Universitätsmedizin Göttingen)
17.00 Concluding remarks: Prof. Dr. Mark Schweda (Carl von Ossietzky Universität Oldenburg)
-----
Abstracts:
Prof. Nancy Jecker, PhD (University of Washington School of Medicine)
As Temperatures Rise, Should Birthrates Fall?: A Parenting Ethics Response to Climate Change
This presentation argues that people in countries with high per capita carbon footprints, generally located in the Global North, should have smaller families. While arithmetic reproductive rates are also important, the focus is reproductive carbon rates, which are generally high in places with low rates of arithmetic reproduction. The presentation’s main argument appeals to two principles: respect for dignified lives, operationalized in terms of a capability view of justice, and fairness, considered from a global standpoint.
Dr. Nitzan Rimon-Zarfaty (Universitätsmedizin Göttingen, Sapir Academic College)
Putting Reproduction on Ice: Navigating Temporality in Social Egg Freezing – A Comparative Study of Germany and Israel
Reproductive decisions concerning temporality and timing are not only individual, but often mirror socially constructed and highly gendered perceptions and expectations. Such perceptions are in turn reflected, negotiated, and challenged in the context of Assistive Reproductive Technologies (ARTs). Initially developed to overcome infertility, ARTs are now also used to control the biology of fertility and its temporality. Cryo-technologies, and particularly "social egg freezing" (SEF), exemplify this trend. SEF enables women to disassociate their reproductive potential from its inherent biological rhythms, rendering it a compelling site for examining the manner in which related temporalities are negotiated. This paper will present cross-cultural comparative findings derived from personal semi-structured interviews with German and Israeli women who have utilized SEF. Analysis revealed different motivations embedded in three predominant temporal notions: First, there is a tendency to postpone reproduction and related decision-making processes by "extending the present," a notion primarily expressed by German interviewees. Second, there is a concept of waiting (for a partner in the context of singlehood), which is prominent in both countries. Third, there is reproductive "futurism" in the form of planning, which is identified among Israeli Jewish-religious interviewees who froze their eggs in the hope of having multiple children. A comparative discussion of these findings is offered in relation to relevant cultural scripts, moral values, and gender imaginaries that navigate the (re)construction of reproductive temporalities.
Funding: This project has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement No. 749889. The project also received funding from the Minerva Stiftung Post-Doctoral Fellowship of the Max Planck Society .
Dr. Isabella Marcinski-Michel (Universitätsmedizin Göttingen) und Prof. Dr. Claudia Wiesemann (Universitätsmedizin Göttingen)
Reproductive Healthcare, Time, and the Good Life
For many, having children and starting a family is an essential aspect of the good life. While for centuries the temporal limitation of reproduction in middle age was taken for granted, at least for women, modern medical innovations, especially in reproductive medicine, seem to make this phase of life an object of planning, control and optimisation. The proverbial “biological clock”, it is promised, could be stopped, reproduction could be made more dynamic in time. Reproductive medicine offers a wide range of techniques such as in vitro fertilisation, in particular reproduction by sperm and egg donation, cryopreservation of gametes, pre-conception, pre-implantation and prenatal diagnostics and, last but not least, abortion and contraception. These techniques make it possible to intervene in the timing of human reproduction, making it more predictable and controllable, and thus accessible to temporal optimisation. Underlying this are implicit or explicit normative concepts of the good life and appropriate temporality, which have so far received comparatively little reflection in medical ethical debates. In this talk, we will examine the temporal distortions and shifts in the life course on the one hand, and the planning and optimisation efforts on the other, with their respective effects on common conceptions of the good life, and evaluate them from an ethical perspective.
Dr. Chris Wareham (Utrecht University)
Cryonics and the Story of a Life: Closing the Book on the Frozen Dead
In Europe and the United States, cryo-preservation of the dead is increasingly common. The aim of cryonics techniques is to preserve the body in the hope that it will one day be possible to repair the damage that led to death. If successful, cryo-preservation and similar biostasis technologies may challenge the conceptualization of death as something that is irreversible.
While it is uncertain that cryonics or other biostasis technologies could be used to resurrect a human, they already present prudential, moral, and medical ethics challenges (Minerva and Sandberg 2017). For the most part, ethical theorists have tended to be in favour of such technologies, arguing that they are permissible (Minerva 2018), prudentially desirable (Shaw 2009), and that there may be ethical duties for states to provide such technologies and even to make them compulsory (Thau 2020).
Proponents of cryonics defuse a host of objections (Hillenbrink and Wareham 2024). However, a neglected consideration is the idea that certainty about death is necessary for a suitable end to life's story. This omission is significant since narrative structure may be an important element of life's meaning and value (Velleman 1991; Anderson 1995; Dorsey 2015). To rectify this I consider the narrative implications of cryonics under conditions of uncertainty, certain failure, and successful resurrection. Drawing on narratives in popular film, fact, and fiction, I make the case that narrative closure should figure prominently in the ethics of cryonics.
Laura Mohacsi (Universitätsmedizin Göttingen) und Lena Stange (Carl von Ossietzky Universität Oldenburg)
Images of Old Age: Bioethics and Perspectives of Health Care Professionals and Seniors
This talk explores the images of old age within bioethical discourse on the one hand, and from the perspectives of healthcare professionals and older adults (aged 75 and older) on the other, focusing on the concept of time and temporality.
Drawing on examples from a narrative review of the bioethical academic discourse and empirical findings from focus group discussions with physicians, nurses, and older adults, as well as individual interviews with older adults (aged 75 and older) with health restrictions, this talk aims to interrogate how time and temporality appears in expressions about “old age”, in both theoretical and practical contexts, and to reflect on the ethical implications of these images for aging individuals and the broader discourse about and understanding of aging.
In bioethics, aging is often framed through narratives of decline, dependency, and finitude, raising critical ethical questions regarding autonomy and care. As key actors in the care and treatment of older people, health care professionals are confronted with these questions in their everyday practice and form their own images of old age in this context. At the same time, their images of old age may influence their approach to patient care. Meanwhile, older adults experience and conceptualize aging from a different perspective, reflecting a range of temporal understandings of their lives, health, and identity.
Prof. Dr. Claudia Dellas (Universitätsmedizin Göttingen)
Chronically Ill with a Congenital Heart Defect. How the Advancements of Medicine Influence the Lives of Those Affected.
Nearly every 100th living newborn is born with a congenital heart defect. Eighty years ago, more than 50% of these children did not survive, most of them died within their first year of life. Thanks to the success in surgical and interventional treatment, more than 90% of these children now reach adulthood. Since the 1990s, this has led to the emergence of a steadily growing new patient group: adults with congenital heart defects (ACHD). Currently, around 300,000 ACHD live in Germany.
This presentation will address the current state of care and the existing medical challenges for these patients. Using the example of their educational and professional opportunities, as well as their ability to form relationships and partnerships, it will highlight the transformation of medical treatment over the past decades—from merely improving survival rates to creating new life chances.
Lisa Nebel (Universitätsmedizin Göttingen) und Annika Freiberger (Deutsches Herzzentrum München)
Parenthood with Chronic Illness: The Importance of Generativity for the Quality of Life in Adults with Congenital Heart Disease
Improved treatment options for congenital heart disease (CHD) lead to a growing number of women with CHD at reproductive age. Due to physical and psychological burden, pregnancies in women with CHD often count for high-risk. Resulting emotional distress can adversely impact pregnancy, motherhood and fetal health. Nevertheless, young women with CHD frequently report a strong desire to have children – with starting a family being perceived as a central component of a fulfilling life. Erik H. Erikson (1973) described the need to contribute to the next generation through reproduction and parenthood as generativity, identifying it as a key developmental task in middle adulthood.
This contribution examines the significance of generativity, particularly parenthood, for young women with CHD. To provide a comprehensive perspective, findings from two quantitative studies conducted at the German Heart Center Munich (DHM) and a qualitative study from the Department of Psychosomatic Medicine and Psychotherapy at University Medical Center Göttingen (UMG) are integrated: (1) A retrospective study at DHM investigated the psychological impact and adaptation indicators in women with CHD before, during and after pregnancy. The novel concept of illness identity was applied to explain how patients experience and integrate their CHD into their identities. Patient-reported outcome measures on mental functioning and illness identity were assessed in a sample of 121 postpartum women with CHD at the German Heart Centre Munich. (2) A second study on bonding and social support was done in a sample of 178 postpartum women with CHD. (3) A qualitative interview study at UMG explored the perspectives of 14 young adults with CHD (aged 19–29) on a good life with AHF and their experiences of temporality. Reproduction and generativity emerged as a central intersection between these phenomena.
Dr. Anne Clausen und Dr. Daniel Broschmann (Universitätsmedizin Göttingen)
Chronic Heart Disease and the Future: the Concept of Existential Possibility
Thanks to advancements in modern medicine, the future prospects for individuals with congenital heart defects have significantly improved over the past few decades, with most affected individuals now reaching advanced adulthood. However, their life possibilities can be constrained by factors such as reduced physical endurance, necessary surgical interventions, regular medical check-ups, and the disciplined management of medications. While achieving typical developmental milestones may be challenging or even unattainable for those with congenital heart defects, a biographical rupture caused by a severe heart condition that manifests in adulthood—such as a heart attack or severe arrhythmia—can lead to a sudden constriction of the horizon of possibility. On the other hand, individuals from both groups report experiences of post-traumatic growth, including a re-evaluation of priorities that favors meaningful relationships, an increased awareness of the present moment, and an earlier onset of "existential maturity" among those with congenital heart defects. The interdisciplinary presentation by Anne Clausen and Daniel Broschmann seeks to explore heart diseases through the lens of the phenomenological concept of "existential possibility," utilizing selected interview excerpts and case studies to investigate the implications of this approach.